Adipose-Derived Stem Cells (ADSCs)
Summary
Adipose-Derived Stem Cells (ADSCs) represent a powerful tool in the field of regenerative medicine, offering immense potential for tissue repair, regeneration, and disease treatment. Their unique properties, including multipotent differentiation capabilities and immunomodulatory effects, make them highly attractive for a wide range of therapeutic applications.
From orthopedic injuries to dermatological conditions, cardiovascular diseases, and neurodegenerative disorders, ADSC-based therapies hold promise for transforming the way we approach healthcare and disease treatment. As research continues to advance and technology evolves, ADSCs are poised to play a central role in shaping the future of regenerative medicine, offering hope to millions of patients worldwide.
Understanding Adipose-Derived Stem Cells (ADSCs)
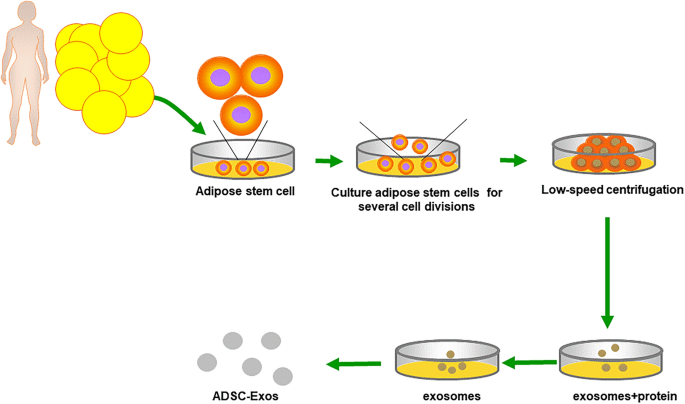
ADSCs are a type of mesenchymal stem cell (MSC) that can be easily isolated from adipose tissue through minimally invasive procedures such as liposuction or lipoaspiration. Unlike embryonic stem cells, ADSCs are derived from adult tissue, bypassing ethical concerns and regulatory hurdles associated with embryonic stem cell research. The abundance of adipose tissue in the body makes ADSCs readily accessible, offering a plentiful and reliable source for therapeutic use.
Characteristics and Properties of ADSCs
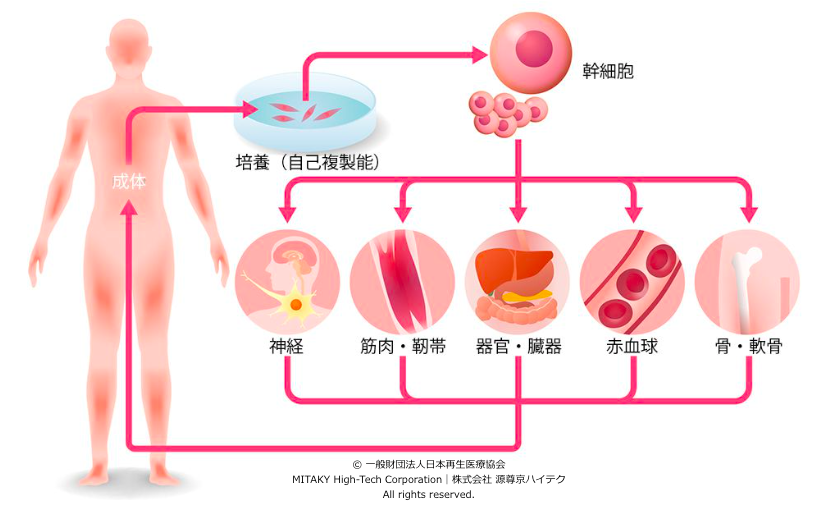
- Multipotent Differentiation: ADSCs have the capacity to differentiate into various cell lineages, including adipocytes, osteoblasts, chondrocytes, and myocytes. This versatility enables ADSCs to contribute to the regeneration of diverse tissues and organs.
- Immunomodulatory Properties: ADSCs exhibit immunomodulatory effects by suppressing inflammatory responses and regulating immune cell activity. This feature is particularly beneficial for treating autoimmune disorders and inflammatory conditions.
- High Proliferative Capacity: ADSCs possess a high proliferation rate, allowing for the generation of large quantities of cells for therapeutic purposes. This scalability is critical for clinical applications requiring substantial cell numbers.
Four Applications of ADSCs in Regenerative Medicine
1. Tissue Regeneration and Repair:
ADSCs hold promise for the regeneration of musculoskeletal tissues, including bone, cartilage, and muscle. Studies have demonstrated the effectiveness of ADSCs in promoting bone healing, accelerating fracture repair, and mitigating cartilage degeneration. ADSC-based therapies offer potential treatments for conditions such as osteoarthritis, osteoporosis, and musculoskeletal injuries, providing alternatives to conventional treatments like joint replacement surgery.
2. Dermatological Applications:
ADSCs play a crucial role in skin regeneration and wound healing. Their ability to stimulate tissue repair, angiogenesis, and collagen synthesis makes them valuable assets in treating chronic wounds, burns, and dermatological conditions. ADSC-based therapies offer potential solutions for improving wound closure rates, reducing scar formation, and enhancing the cosmetic outcomes of reconstructive procedures.
3. Orthopedic Medicine:
ADSCs hold promise for cardiac regeneration and repair following myocardial infarction (MI). Studies have shown that ADSC transplantation can improve cardiac function, reduce scar formation, and stimulate angiogenesis in animal models of MI. ADSC-based therapies offer potential treatments for heart failure, ischemic heart disease, and other cardiovascular conditions, providing hope for patients with limited treatment options.
4. Neurological Disorders and Injury Repair:
ADSCs offer potential treatments for neurological disorders and injuries, including stroke, spinal cord injury, and neurodegenerative diseases. Preclinical studies have shown that ADSC transplantation can promote neurogenesis, enhance neuronal survival, and improve functional recovery in animal models of neurological damage. ADSC-based therapies hold promise for restoring neurological function and improving quality of life for patients with debilitating conditions.
Challenges and Future Directions
Despite the significant progress in ADSC research, several challenges remain to be addressed. Standardization of isolation and culture protocols is essential to ensure the consistency and safety of ADSC-based therapies. Moreover, the long-term safety and efficacy of these therapies need to be rigorously evaluated through clinical trials to establish their viability as mainstream treatment options.
In addition, regulatory frameworks governing the use of ADSCs in regenerative medicine must be established to ensure ethical and responsible practices. The ethical considerations surrounding stem cell research, including issues of informed consent, patient safety, and equitable access to treatment, must be carefully addressed to foster public trust and confidence in this emerging field.
Looking ahead, the future of ADSCs in regenerative medicine appears promising, with ongoing research efforts focused on refining techniques, optimizing protocols, and exploring new therapeutic avenues. Advances in stem cell technology, tissue engineering, and gene editing hold the potential to further enhance the therapeutic capabilities of ADSCs and revolutionize the landscape of regenerative medicine.
Powered by MITAKY High-Tech Corporation|株式会社 源尊京ハイテク
Citations:
- Huang, J. I., & Zuk, P. A. (2002). Adipose-derived stem cells: a new source for musculoskeletal regeneration. Journal of the American College of Surgeons, 195(3), 329-334.
- Rigotti, G., Marchi, A., Galie, M., Baroni, G., Benati, D., Krampera, M., … & Sbarbati, A. (2007). Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plastic and reconstructive surgery, 119(5), 1409-1422.
- Cai, L., Johnstone, B. H., Cook, T. G., Tan, J., Fishbein, M. C., Chen, P. S., & March, K. L. (2009). IFATS collection: Human adipose tissue-derived stem cells induce angiogenesis and nerve sprouting following myocardial infarction, in conjunction with potent preservation of cardiac function. Stem cells, 27(1), 230-237.
- Cui, L., Jiang, J., Wei, L., Zhou, X., Fraser, J. L., Snider, B. J., … & Lu, M. (2007). Transplantation of embryonic stem cells improves nerve repair and functional recovery.